Diabetes Mellitus
Obesity is a major independent risk factor for developing type 2 diabetes, and more than 90% of type 2 diabetics are overweight or obese.
It has been estimated that the risk of developing Type 2 diabetes is increased 93-fold in women and 42-fold in men who are severely obese rather than of healthy weight.
Diabetes is the leading cause of kidney failure, non-traumatic lower-limb amputations, new cases of blindness among adults, and it is associated with increased risk of: heart disease and stroke, high blood pressure, nervous system disease, kidney disease, blindness, amputations, pregnancy complications.
Roux-en-Y gastric bypass and sleeve gastrectomy are effective interventions for treating type 2 diabetes. Improvement in metabolic control is often evident within days to weeks following surgery, most likely reflecting an alteration in metabolism that is independent of weight loss.
2011 statement from International Diabetes Federation said that bariatric surgery can significantly improve glycaemic control in severely obese patients with Type 2 diabetes. It is an effective, safe and cost-effective therapy for obese Type 2 diabetes. Surgery can be considered an appropriate treatment for people with Type 2 diabetes and obesity not achieving recommended treatment targets with medical therapies, especially in the presence of other major co-morbidities.
Fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease worldwide, and morbid obesity is strongly associated with its development. NAFLD is subdivided into nonalcoholic fatty liver (NAFL), hepatic steatosis without inflammation, and nonalcoholic steatohepatitis (NASH), which is associated with inflammation and can be indistinguishable histologically from alcoholic steatohepatitis.
The general approach to the overweight or obese patient with NAFLD or NASH is lifestyle modification and weight loss.
Although it was a rare indication for liver transplant 20 years ago, NSAH now is No.2 reason for people to get liver transplant. It is estimated that it will be the No.1 reason for liver transplant in the near future with the epidemics of obesity.
There is no good treatment for NASH except weight lose. Bariatric surgery has been shown to be the most effective ways to slow down or reverse the progression of NASH. Studies have shown more than 80% of resolution of NASH after bariatric surgery.
Hypertension and Hyperlipidemia
The Framingham Heart Study estimated that overweight and obesity accounted for approximately 26 percent of cases of hypertension in men and 28 percent in women and for approximately 23 percent of cases of coronary heart disease in men and 15 percent in women.
Bariatric surgery was reported to cause normalization of hypertension in 30-50% of patients with medication and reduced need of antihypertensive treatment in a further 20-30% of patients.
Patients with complete resolution of hypertension after surgery usually had a shorter duration of hypertension compared with patients without resolution. That means the sooner to have bariatric surgery, the better chance to have remission of hypertension for obese patients.
Up to 50% of morbidly obese patients who undergo bariatric surgery have dyslipidemia.
Large studies show that bariatric surgery leads to resolution of dyslipidemia in about 60% of the patients.
Meta analysis showed that bariatric surgery leads to close to 50% reduction of heart attack risk and more than 50% reduction of stroke risk.
Joint Pain and Osteoarthritis (OA)
The Knee osteoarthritis risk was 0.1% for BMI < 20, but 13.6% for BMI> 36. For every 5kg weight gain, there is a commensurate 36% increased risk for developing OA.
The relative risk for women with a BMI > 30 requiring joint replacement compared with BMI
Mortality
Large epidemiologic studies showed that obesity is associated with higher chance of dying early.
A prospective study from the United States revealed an increased risk of death with being either overweight (20 to 50 percent increase in those between 26.5 to 29.9) or obese (two- to over threefold increase in those ≥30).
An analysis of 57 prospective studies with more than 894,000 European and North American adults demonstrated that mortality was lowest among men and women with a BMI between 22.5 to 25, and there was a 30 percent increase in overall mortality for each 5 increase in BMI.
Bariatric surgery has been shown by many studies in Europe and North America to reduce the chance of dying in the long term.
A retrospective cohort study in Utah with more than 7,000 patients showed a 40% reduction in all-cause mortality with 7 years of follow up.
Recently a large study from VA showed more than 50% reduction of mortality with 5-10 years of follow up.
A Canadian study showed that bariatric surgery resulted in 89% reduction of mortality.
Giving the dramatically improved safety of bariatric surgery in the past 10 years, not having surgery is more dangerous than having surgery for morbidly obese patients in the long term.
Obstructive Sleep Apnea
In both males and females, the strongest risk factor for OSA is obesity. A 10 percent increase in weight was associated with a six fold increase in risk of incident OSA In a population-based study of over 1000 adults, moderate to severe OSA was present in 11 percent of men who were normal weight, 21 percent of those who were overweight (BMI 25 to 30 kg/m2), and 63 percent of those who were obese (BMI >30 kg/m2)
Weight loss and continuous positive airway pressure (CPAP) therapy are the cornerstones of therapy for
sleep apnea.
A meta-analysis of 69 studies and 13,900 obese patients performed in 2013 identified a high rate of resolution or improvement in OSA following bariatric procedures. The study found that resolution or improvement of OSA for happened in 79% of patient who had Roux-en-Y gastric bypass surgery, 77% of patients who had lap band, and 86% of patients who had sleeve gastrectomy.
Obesity Associated Cancer
Large epidemiology studies have shown that obesity confers an increased risk to various malignancies including cancers of the colon, gallbladder, endometrium, breast and pancreas.
In a prospectively studied population of more than 900,000 U.S. adults with 16 years of follow-up, obese men had 52 percent higher chance of dying from cancer, while obese women had 62 percent higher chance of dying of cancer, compared with normal weight men and women. The authors estimated that overweight and obesity in the United States could account for 14 percent of all deaths from cancer in men and 20 percent of those in women.
A recent meta-analysis of 82 studies including more than 200,000 patients with breast cancer demonstrated a 75% increase in mortality in premenopausal women and a 34% increase in mortality in postmenopausal women who were obese at the time of breast cancer diagnosis, as compared with patients who were of normal weight at diagnosis.
Bariatric surgery has been shown to reduce the risk of developing new cancers.
A retrospective cohort study from Utah found 40% decrease of all cause mortality and 60% decrease of cancer related mortality
A large retrospective study from Canada showed nearly 80% reduction of cancer incidence after bariatric surgery.
Polycystic Ovary Syndrome and Infertility
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder in women. It is strongly associated with obesity. It is found in 30 percent to 70 percent of obese women of reproductive age and is associated with irregular period, excessive hair and a high risk of infertility.
Studies have shown that most obese women who effectively achieved weight loss following a Roux-en-Y gastric bypass had restored menstrual cycles, marked improvement of excessive hair and decreased androgen level.
For PCOS patients with infertility, bariatric surgery also has been shown to increase the fertility rate.
Even in women with regular menstrual period, observational studies have shown obesity is associated with decreased spontaneous pregnancy rates and increased time to pregnancy.
Studies from Italy, Canada and United States all showed that bariatric surgery significantly increased the fertility rate in obese women.
A retrospective study in Italy involving 110 obese women who tried unsuccessfully to become pregnant before bariatric surgery. After surgery, 69 became pregnant. No pregnancy related complications were found.
A large study from Canada involving 783 obese women showed that 47.0% of patients who were unable to become pregnant preoperatively were successful after bariatric surgery.
Quality of Life
Obesity is associated with impairments in quality of life. In particular, obesity can cause increased physical limitations, bodily pain, and fatigue.
psychosocial function
Numerous studies have suggested that individuals report improvements in psychosocial functioning with weight reduction. The most consistent finding in this area is the association between surgical weight loss* and improved quality of life.
Life expectancy
Obese patients who had bariatric surgery not only live longer, but also live much better.
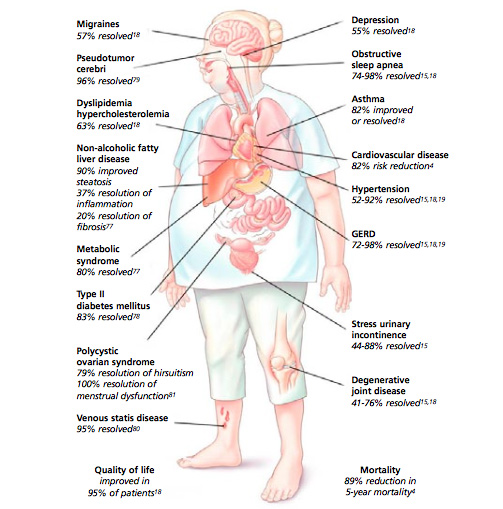
Percentage of conditions resolved after bariatric surgery.
Explore our weight loss procedures
Calculate your BMI
The Body Mass Index (BMI) is a measure for human body shape based on an individual's height and weight.
